Vasodilator Drugs
Therapeutic Use and Rationale
Therapeutic Uses of
Vasodilators
- Systemic and pulmonary
hypertension - Heart failure
- Angina
As the name implies, vasodilator drugs relax the smooth muscle in blood vessels, which causes the vessels to dilate. Dilation of arterial (resistance) vessels leads to a reduction in systemic vascular resistance, which reduces arterial blood pressure. Dilation of venous capacitance vessels decreases venous blood pressure.
Vasodilators are used to treat hypertension, heart failure and angina; however, some vasodilators are better suited than others for these indications. For example, vasodilators that act primarily on resistance vessels (arterial dilators) are used for hypertension, heart failure, and angina; however, reflex cardiac stimulation makes some arterial dilators unsuitable for angina. Venous dilators are very effective for angina, and sometimes used for heart failure, but are not used as primary therapy for hypertension unless a particular drug also causes arterial dilation (mixed vasodilator). Most vasodilator drugs are mixed (or balanced) vasodilators in that they dilate both arteries and veins and therefore can have wide application in hypertension, heart failure and angina. Some vasodilators, because of their mechanism of action, also have other important actions that can sometimes enhance their therapeutic utility or provide some additional therapeutic benefit. For example, some calcium channel blockers not only dilate blood vessels but also depress cardiac mechanical and electrical function, which can enhance their antihypertensive actions and confer additional therapeutic benefits, such as blocking arrhythmias.
Arterial dilators
Arterial dilator drugs are commonly used to treat systemic and pulmonary hypertension, heart failure and angina. They reduce arterial pressure by decreasing systemic vascular resistance. This benefits patients in heart failure by reducing the afterload on the left ventricle, which enhances stroke volume and cardiac output and leads to secondary decreases in ventricular preload and venous pressures. Anginal patients benefit from arterial dilators because by reducing ventricular afterload, arterial vasodilators decrease the oxygen demand of the heart, and improve the oxygen supply/demand ratio. Oxygen demand is reduced because ventricular wall stress is reduced when aortic pressure is decreased. Some vasodilators can also reverse or prevent arterial vasospasm (transient contraction of arteries), which can precipitate anginal attacks.
Although most drugs that dilate arteries also dilate veins, hydralazine, a direct acting vasodilator, is highly selective for arterial resistance vessels.
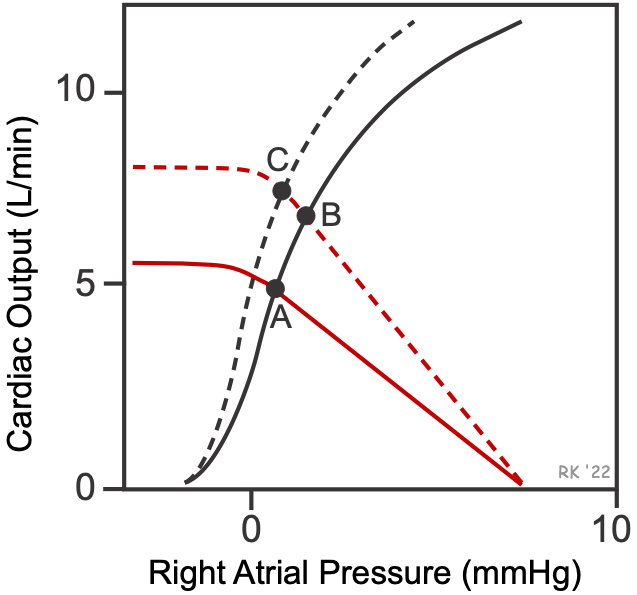 The effects of arterial dilators on overall cardiovascular function can be depicted graphically using cardiac and systemic vascular function curves as shown in the figure. Selective arterial dilation decreases systemic vascular resistance, which increases the slope of the systemic vascular function curve (red dashed line) without appreciably changing the x-intercept (mean circulatory filling pressure). This alone causes the operating point to shift from A to B, resulting in an increase in cardiac output with a small increase in right atrial pressure. The reason for the increase in right atrial pressure is that arterial dilation increases blood flow from the arterial vasculature into the venous vasculature, increasing venous volume and pressure. However, arterial dilators also reduce afterload on the left ventricle and therefore unload the heart, which enhances the pumping ability of the heart. This causes the cardiac function curve (black dashed line) to shift up and to the left (see point C). Adding to this afterload effect is the influence of enhanced sympathetic stimulation because of a baroreceptor reflex in response to the fall in arterial pressure, which increases heart rate and inotropy. Because of these compensatory cardiac responses, arterial dilators increase cardiac output with little or no change in right atrial pressure (cardiac preload). Although cardiac output is increased, systemic vascular resistance is reduced relatively more, causing arterial pressure to fall. The effect of reducing afterload on enhancing cardiac output is even greater in failing hearts because stroke volume is more sensitive to the influence of elevated afterload in hearts with impaired contractility.
The effects of arterial dilators on overall cardiovascular function can be depicted graphically using cardiac and systemic vascular function curves as shown in the figure. Selective arterial dilation decreases systemic vascular resistance, which increases the slope of the systemic vascular function curve (red dashed line) without appreciably changing the x-intercept (mean circulatory filling pressure). This alone causes the operating point to shift from A to B, resulting in an increase in cardiac output with a small increase in right atrial pressure. The reason for the increase in right atrial pressure is that arterial dilation increases blood flow from the arterial vasculature into the venous vasculature, increasing venous volume and pressure. However, arterial dilators also reduce afterload on the left ventricle and therefore unload the heart, which enhances the pumping ability of the heart. This causes the cardiac function curve (black dashed line) to shift up and to the left (see point C). Adding to this afterload effect is the influence of enhanced sympathetic stimulation because of a baroreceptor reflex in response to the fall in arterial pressure, which increases heart rate and inotropy. Because of these compensatory cardiac responses, arterial dilators increase cardiac output with little or no change in right atrial pressure (cardiac preload). Although cardiac output is increased, systemic vascular resistance is reduced relatively more, causing arterial pressure to fall. The effect of reducing afterload on enhancing cardiac output is even greater in failing hearts because stroke volume is more sensitive to the influence of elevated afterload in hearts with impaired contractility.
To summarize, arterial vasodilators:
- Decrease systemic vascular resistance
- Reduce arterial pressure
- Enhance cardiac output by reducing ventricular afterload
- Improve blood flow to many organs
- Increase central venous pressure
- Elicit baroreflex-mediated cardiac stimulation
Venous dilators
Drugs that dilate venous capacitance vessels serve two primary functions in treating cardiovascular disorders:
- Venous dilators reduce venous pressure, which reduces preload on the heart, decreasing cardiac output. This is useful in angina because it decreases the oxygen demand of the heart and increases the oxygen supply/demand ratio. Oxygen demand is reduced because decreasing preload leads to a reduction in ventricular wall stress by decreasing the size of the heart.
- Reducing venous pressure decreases proximal capillary hydrostatic pressure, which reduces capillary fluid filtration and edema formation. Therefore, venous dilators are sometimes used in the treatment of heart failure along with other drugs because they help to reduce pulmonary and systemic edema that results from the heart failure.
Although many vasodilator drugs dilate veins and arteries, some drugs, such as organic nitrate dilators, are relatively selective for veins.
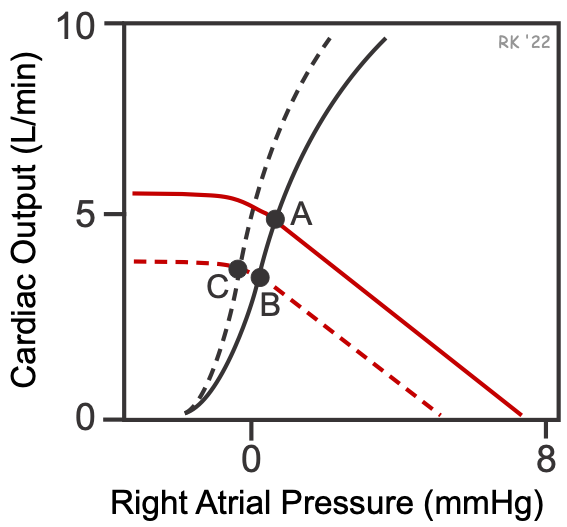 The effects of selective venous dilators on overall cardiovascular function in normal subjects can be depicted graphically using cardiac and systemic vascular function curves, as shown in the figure. Venous dilation increases venous compliance by relaxing the venous smooth muscle. Increased compliance causes a downward parallel shift to the left of the vascular function curve (dashed red line), which decreases the mean circulatory filling pressure (x-intercept). This causes the operating point to shift from A to B, resulting in a decrease in cardiac output with a small decrease in right atrial pressure. The reason for these changes is that venous dilation, by reducing right atrial pressure, decreases right ventricular preload, which decreases stroke volume and cardiac output by the Frank-Starling mechanism. Reduced cardiac output causes a fall in arterial pressure, which reduces afterload on the left ventricle and leads to baroreceptor reflex responses, both of which can shift the cardiac function curve up and to the left (black dashed line). Sympathetic activation can also lead to an increase in systemic vascular resistance (not shown in the figure). The cardiac effects (decreased cardiac output) of venous dilation are more pronounced in normal hearts than in failing hearts because of where the hearts are operating on their Frank-Starling curves (cardiac function) curves (click here for more information).
The effects of selective venous dilators on overall cardiovascular function in normal subjects can be depicted graphically using cardiac and systemic vascular function curves, as shown in the figure. Venous dilation increases venous compliance by relaxing the venous smooth muscle. Increased compliance causes a downward parallel shift to the left of the vascular function curve (dashed red line), which decreases the mean circulatory filling pressure (x-intercept). This causes the operating point to shift from A to B, resulting in a decrease in cardiac output with a small decrease in right atrial pressure. The reason for these changes is that venous dilation, by reducing right atrial pressure, decreases right ventricular preload, which decreases stroke volume and cardiac output by the Frank-Starling mechanism. Reduced cardiac output causes a fall in arterial pressure, which reduces afterload on the left ventricle and leads to baroreceptor reflex responses, both of which can shift the cardiac function curve up and to the left (black dashed line). Sympathetic activation can also lead to an increase in systemic vascular resistance (not shown in the figure). The cardiac effects (decreased cardiac output) of venous dilation are more pronounced in normal hearts than in failing hearts because of where the hearts are operating on their Frank-Starling curves (cardiac function) curves (click here for more information).
Therefore, the cardiac and vascular responses to venous dilation are complex when both direct effects and indirect compensatory responses are considered. The most important effects in terms of clinical utility for patients are summarized below.
To summarize, venous dilators:
- Decrease venous pressure
- Reduce cardiac output by decreasing preload
- Decrease arterial pressure
- Reduce myocardial oxygen demand
- Decrease capillary fluid filtration and tissue edema
Mixed or "balanced" dilators
The effects of mixed dilators on cardiac and vascular function depend on the relative arterial and venous dilation. Mixed vasodilators decrease systemic vascular resistance and arterial pressure, with relatively little change in right atrial (or central venous) pressure. The venous dilation (reduced cardiac preload) also partially offsets the cardiac output enhancing effects of reduced afterload. This contrasts with a pure arterial vasodilator that lowers arterial pressure and increases venous pressure a small amount, which leads to a greater increase in cardiac output.
Side Effects of Vasodilators
There are three potential drawbacks to the use of vasodilators:
- Systemic vasodilation and arterial pressure reduction can lead to a baroreceptor-mediated reflex stimulation of the heart (increased heart rate and inotropy). This increases oxygen demand, which is undesirable if the patient also has coronary artery disease.
- Vasodilators can impair normal baroreceptor-mediated reflex vasoconstriction when a person stands up, which can lead to orthostatic hypotension and syncope upon standing.
- Vasodilators can lead to renal retention of sodium and water, which increases blood volume and cardiac output and compensates for the reduced systemic vascular resistance.
Drug Classes and General Mechanisms of Action
Vasodilator drugs can be classified based on their site of action (arterial vs. venous) or by the mechanism of action. Some drugs primarily dilate resistance vessels (arterial dilators; e.g., hydralazine), while others primarily affect venous vessels (venous dilators; e.g., nitroglycerin). Most vasodilator drugs, however, have mixed arterial and venous dilator properties (mixed dilators; e.g., alpha-adrenoceptor antagonists, angiotensin converting enzyme inhibitors).
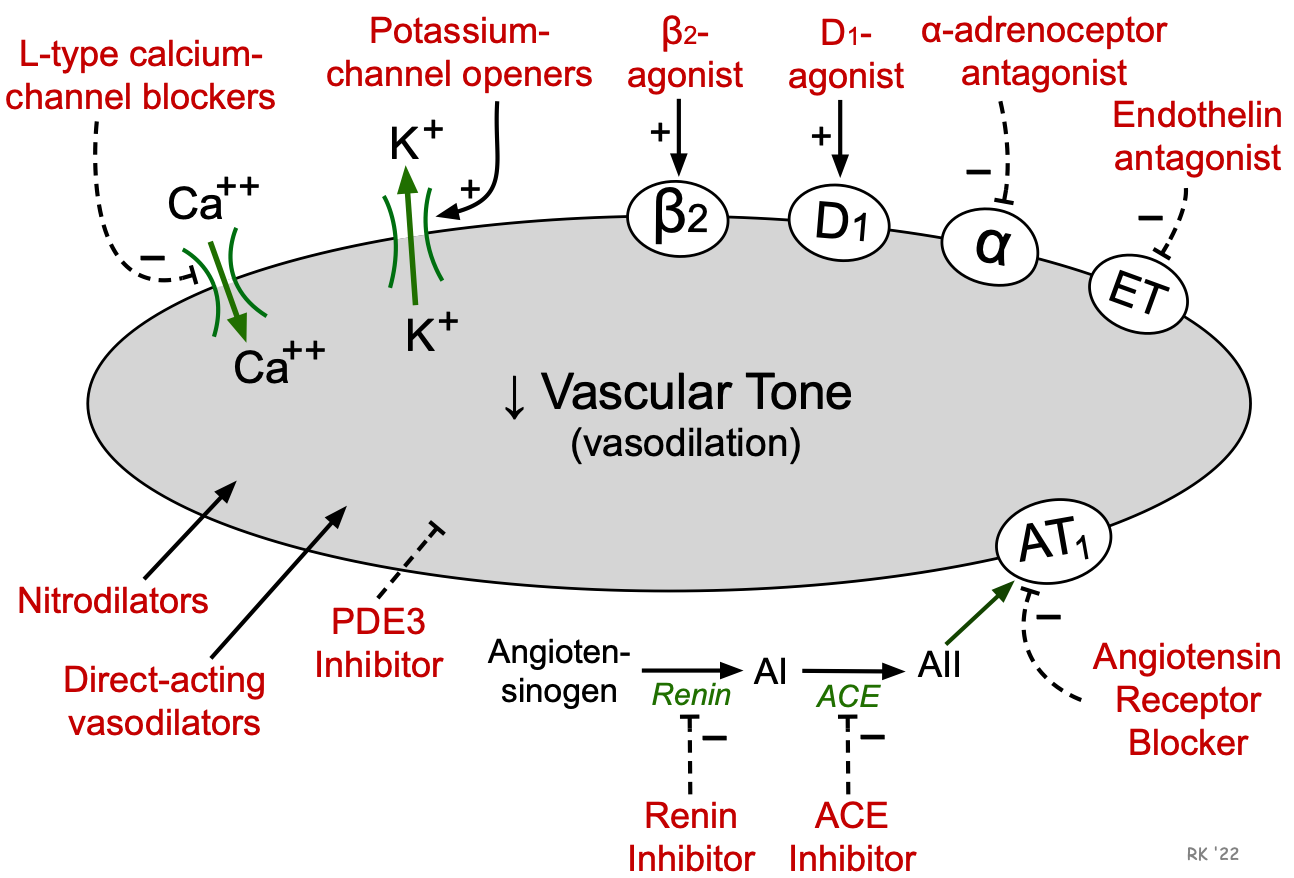
It is more common, however, to classify vasodilator drugs based on their primary mechanism of action (e.g., alpha-blocker, angiotensin receptor blocker). The figure depicts important mechanistic classes with vasodilator properties. Note that some drugs in the following list are not referred to as vasodilators despite having that property because of other effects such as cardiac stimulation (e.g., beta-agonists are cardiotonic drugs because of beta1-agonist properties, although their beta2 properties produce vasodilation). Dopamine possesses dopaminergic (D1) agonist properties and therefore produces vasodilation at low concentrations; however, it also has beta1- and alpha-adrenoceptor agonist properties that can cause cardiac stimulation and vasoconstriction at high plasma concentrations. Other drugs, such as centrally acting sympathomimetics and ganglionic blockers, do not act directly on vessels, but produce vasodilation by inhibiting sympathetic efferent activity to blood vessels. Click on the drug class for more details.
- Alpha-adrenoceptor antagonists (alpha-blockers)
- Angiotensin converting enzyme (ACE) inhibitors
- Angiotensin receptor blockers (ARBs)
- Beta2-adrenoceptor agonists (β2-agonists)
- Calcium-channel blockers (CCBs)
- Centrally acting sympatholytics
- Direct acting vasodilators
- Dopamine agonists
- Endothelin receptor antagonists
- Ganglionic blockers
- Nitrodilators
- Phosphodiesterase inhibitors
- Potassium-channel openers
- Renin inhibitors
Revised 11/30/2023
 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)