Alpha-Adrenoceptor Antagonists (Alpha-Blockers)
General Pharmacology
These drugs block the effect of sympathetic nerves on blood vessels by binding to alpha-adrenoceptors on the vascular smooth muscle. Most of these drugs act as competitive antagonists to the binding of norepinephrine that is released by sympathetic nerves synapsing on smooth muscle. Therefore, these drugs are sometimes referred to as sympatholytics because they antagonize sympathetic activity. Some alpha-blockers are non-competitive (e.g., phenoxybenzamine), which prolongs their action because of their strong binding to the receptor.
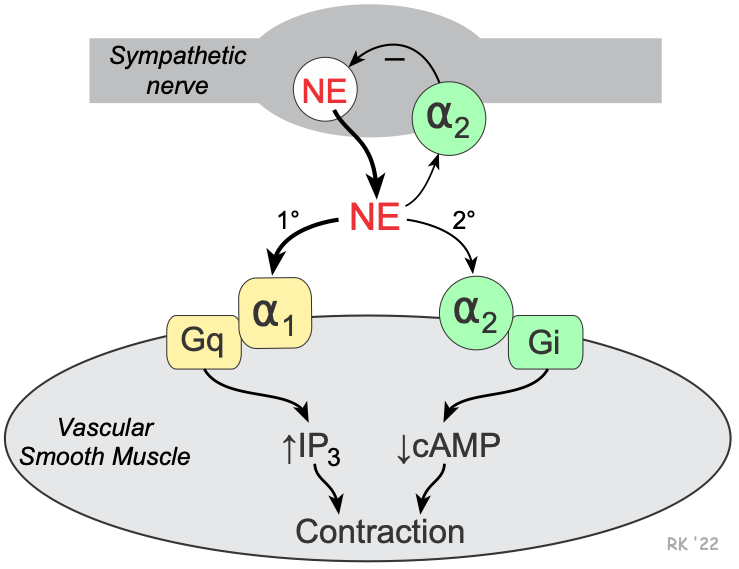 Vascular smooth muscle has two types of alpha-adrenoceptors: alpha1 (α1) and alpha2 (α2). The α1-adrenoceptors are the predominant α-receptors on vascular smooth muscle. These receptors are linked to Gq-proteins that activate smooth muscle contraction through the IP3 signal transduction pathway. Depending on the tissue and type of vessel, there are also α2-adrenoceptors found on the smooth muscle. These receptors are linked to Gi-proteins, and binding of an alpha-agonist to these receptors decreases intracellular cAMP, which causes smooth muscle contraction. There are also α2-adrenoceptors on the sympathetic nerve terminals that inhibit the release of norepinephrine and therefore act as a negative feedback mechanism for modulating the release of norepinephrine.
Vascular smooth muscle has two types of alpha-adrenoceptors: alpha1 (α1) and alpha2 (α2). The α1-adrenoceptors are the predominant α-receptors on vascular smooth muscle. These receptors are linked to Gq-proteins that activate smooth muscle contraction through the IP3 signal transduction pathway. Depending on the tissue and type of vessel, there are also α2-adrenoceptors found on the smooth muscle. These receptors are linked to Gi-proteins, and binding of an alpha-agonist to these receptors decreases intracellular cAMP, which causes smooth muscle contraction. There are also α2-adrenoceptors on the sympathetic nerve terminals that inhibit the release of norepinephrine and therefore act as a negative feedback mechanism for modulating the release of norepinephrine.
Alpha1-adrenoceptor antagonists cause vasodilation by blocking the binding of norepinephrine to the smooth muscle receptors. Non-selective α1 and α2-adrenoceptor antagonists block postjunctional α1 and α2-adrenoceptors, which causes vasodilation; however, the blocking of prejunctional α2-adrenoceptors leads to increased release of norepinephrine, which attenuates the effectiveness of the α1 and α2-postjunctional adrenoceptor blockade. Blocking α2-prejunctional adrenoceptors in the heart can lead to increases in heart rate and contractility because of the enhanced release of norepinephrine that binds to beta1-adrenoceptors.
Alpha-blockers dilate both arteries and veins because both vessel types are innervated by sympathetic adrenergic nerves; however, the vasodilator effect is more pronounced in the arterial resistance vessels. Because most blood vessels have some sympathetic tone under basal conditions, these drugs are effective dilators. They are even more effective under conditions of elevated sympathetic activity (e.g., during stress) or during pathologic increases in circulating catecholamines caused by an adrenal gland tumor (pheochromocytoma).
Therapeutic Uses
Selective α1-blockers are used in the treatment of primary hypertension, although their use is not as widespread as other antihypertensive drugs. Alpha1-blockers are not recommended as monotherapy, and therefore are used with other antihypertensive drugs. Non-selective antagonists are usually reserved for hypertensive emergencies caused by a pheochromocytoma. This hypertensive condition, which is most commonly caused by an adrenal gland tumor that secretes large amounts of catecholamines. It is commonly managed by a non-selective alpha-blocker in addition to a beta-blocker (to blunt the reflex tachycardia) until the tumor can be surgically removed.
Specific Drugs
Alpha-blockers used in treating essential hypertension are all highly selective for α1-adrenoceptors. Non-selective blockers are used during hypertensive crisis caused by elevated circulating catecholamines (pheochromocytoma). The following table compares different alpha-blockers that are presently used in patients.
Alpha-blocker type | Specific Drugs | Comments |
Selective | prazosin | prototypical drug; essential hypertension; T1/2 is ~ 3 hours |
| terazosin | essential hypertension; T1/2 is ~ 12 hours | |
| doxazosin | essential hypertension; T1/2 is ~ 20 hours | |
Non-selective | phenoxybenzamine | long-lasting non-competitive blockade; T1/2 is ~24 hours; used for hypertension caused by pheochromocytoma |
| phentolamine | used occasionally for hypertension caused by pheochromocytoma |
Side Effects and Contraindications
The most common side effects are related directly to alpha-adrenoceptor blockade. These side effects include dizziness, orthostatic hypotension (because of loss of reflex vasoconstriction upon standing), nasal congestion (because of dilation of nasal mucosal arterioles), headache, and reflex tachycardia (especially with non-selective alpha-blockers). Fluid retention is also a problem that can be rectified by co-administration of a diuretic with the alpha-blocker. Alpha blockers have not been proven to be beneficial in heart failure or angina, and should not be used in these conditions.
Revised 11/23/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)