Ganglionic Blockers
Autonomic Ganglia
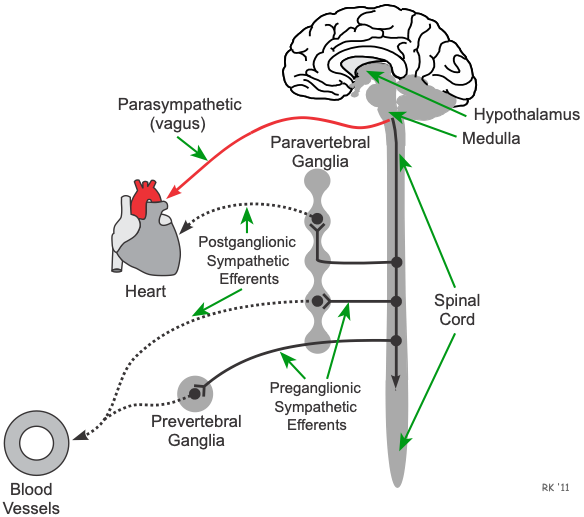 Sympathetic autonomic ganglia are found in the paravertebral ganglia (sympathetic chain ganglia) and the prevertebral ganglia. Preganglionic sympathetic fibers that exit the spinal cord synapse within these ganglia and release the neurotransmitter acetylcholine (ACh), which binds to nicotinic receptors. Activation of the nicotinic receptors depolarizes the cell body of the postganglionic neuron and generates action potentials that travel to the target organ to elicit a response.
Sympathetic autonomic ganglia are found in the paravertebral ganglia (sympathetic chain ganglia) and the prevertebral ganglia. Preganglionic sympathetic fibers that exit the spinal cord synapse within these ganglia and release the neurotransmitter acetylcholine (ACh), which binds to nicotinic receptors. Activation of the nicotinic receptors depolarizes the cell body of the postganglionic neuron and generates action potentials that travel to the target organ to elicit a response.
Parasympathetic autonomic ganglia are found within the target organ. With the vagal nerves that exit the brainstem, their long preganglionic fibers enter the target organ (e.g., heart) where they synapse with postganglionic neurons within small ganglia. Like the sympathetic ganglia, the neurotransmitter is ACh, and it binds to nicotinic receptors to activate the short postganglionic fibers that lie near the target tissue (e.g., sinoatrial node).
General Pharmacology
Sympatholytic drugs can block the sympathetic adrenergic system are three different levels. First, peripheral sympatholytic drugs such as alpha receptor antagonists and beta receptor antagonists block the influence of norepinephrine at the effector organ (heart or blood vessel). Second, there are ganglionic blockers that block impulse transmission at the sympathetic ganglia. Third, there are drugs that block sympathetic activity within the brain. These are called centrally acting sympatholytic drugs.
Neurotransmission within the sympathetic and parasympathetic ganglia involves the release of acetylcholine from preganglionic efferent nerves, which binds to nicotinic receptors on the cell bodies of postganglionic efferent nerves. Ganglionic blockers inhibit autonomic activity by interfering with neurotransmission within autonomic ganglia. This reduces sympathetic outflow to the heart, decreasing cardiac output by decreasing heart rate and contractility. Reduced sympathetic output to the vasculature decreases sympathetic vascular tone, which causes vasodilation and reduced systemic vascular resistance, which decreases arterial pressure. Ganglionic blockers also reduce parasympathetic outflow.
Therapeutic Indications
Ganglionic blockers are not used in the treatment of chronic hypertension because of their side effects and because there are many more effective and safer antihypertensive drugs that can be used. They are, however, occasionally used for hypertensive emergencies.
Specific Drugs
Ganglionic blockers are rarely used clinically because of excessive side effects related to ganglionic blockade of autonomic function. One compound (mecamylamine) is occasionally used in hypertensive emergencies or for producing controlled hypotension during surgery.
Side Effects and Contraindications
Side effects of ganglionic blockers include prolonged neuromuscular blockade and potentiation of neuromuscular blocking agents. It can produce excessive hypotension and impotence because of its sympatholytic effect, and constipation, urinary retention, dry mouth because of its parasympatholytic effect. It also stimulates histamine release.
Revised 11/30/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)