Endothelin Receptor Antagonists
General Pharmacology
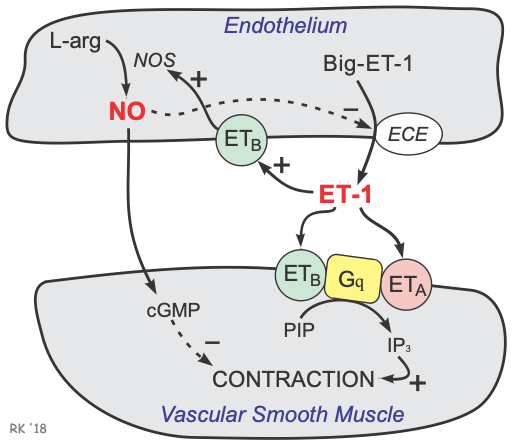 Endothelin-1 (ET-1) is a 21 amino acid peptide that is produced by the vascular endothelium (click here for details). It is a very potent vasoconstrictor that binds to smooth muscle endothelin receptors, of which there are two subtypes: ETA and ETB receptors. These receptors are coupled to a Gq-protein and receptor activation leads to the formation of IP3, which causes the release of calcium by the sarcoplasmic reticulum (SR) and increased smooth muscle contraction and vasoconstriction. There are also ETB receptors on the endothelium that stimulate the formation of nitric oxide, which produces vasodilation in the absence of smooth muscle ETA and ETB receptor activation. This receptor distribution helps to explain the phenomenon that ET-1 administration causes transient vasodilation (initial endothelial ETB activation) and hypotension, followed by prolong vasoconstriction (smooth muscle ETA and ETB activation) and hypertension.
Endothelin-1 (ET-1) is a 21 amino acid peptide that is produced by the vascular endothelium (click here for details). It is a very potent vasoconstrictor that binds to smooth muscle endothelin receptors, of which there are two subtypes: ETA and ETB receptors. These receptors are coupled to a Gq-protein and receptor activation leads to the formation of IP3, which causes the release of calcium by the sarcoplasmic reticulum (SR) and increased smooth muscle contraction and vasoconstriction. There are also ETB receptors on the endothelium that stimulate the formation of nitric oxide, which produces vasodilation in the absence of smooth muscle ETA and ETB receptor activation. This receptor distribution helps to explain the phenomenon that ET-1 administration causes transient vasodilation (initial endothelial ETB activation) and hypotension, followed by prolong vasoconstriction (smooth muscle ETA and ETB activation) and hypertension.
ET-1 receptors in the heart are also linked to the Gq-protein and IP3 signal transduction pathway (click here for details). Therefore, ET-1 in the heart causes the SR to release calcium, which increases contractility. ET-1 also increases the heart rate.
ET-1 can also stimulate cardiac and vascular remodeling, sympathetic activation, and increased aldosterone synthesis.
Therapeutic Indications
Because of its powerful vasoconstrictor properties, and its effects on intracellular calcium, ET-1 has been implicated in the pathogenesis of hypertension, coronary vasospasm, and heart failure. Many studies suggest a role for ET-1 in idiopathic pulmonary hypertension, as well as in systemic hypertension. ET-1 is released by the failing myocardium, where it may contribute to cardiac calcium overload and hypertrophy.
Endothelin receptor antagonists, by blocking the vasoconstrictor and cardiotonic effects of ET-1, produce vasodilation and cardiac inhibition. Endothelin receptor antagonists have been shown to decrease mortality and improve hemodynamics in experimental models of heart failure.
Endothelin antagonists are approved for treatment of pulmonary hypertension and systemic hypertension.
Specific Drugs
Bosentan, a non-selective ET-1 receptor antagonist (blocks ETA and ETB receptors) is currently used in the treatment of pulmonary hypertension; it has a relatively short half-life of 5 hours. In contrast, macitentan is a similar non-selective antagonist, but with a longer half-life (~16 hours; ~48 hours for active metabolite) than bosentan. Another drug also used for pulmonary hypertension is ambrisentan, which is a selective ETA receptor antagonist and has a half-life of about 15 hours.
A new drug, aprocitentan, is approved for treating systemic hypertension. It is a non-selective ET-1 antagonist that is used in combination with other antihypertensive drugs when those drugs cannot adequately control pressure. It has a long half-life (~40 hours) and therefore is only administered once-a-day.
Side Effects and Contraindications
Some endothelin antagonist side effects are common to most vasodilators; namely, headache, cutaneous flushing, and peripheral edema. Hepatotoxicity can also occur. This class of drugs may cause birth defects and therefore is contraindicated in pregnancy. These drugs can also cause liver injury.
Revised 04/27/2024

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)