2023 Redesign Sample Page
This is a Sub-Heading
- THIS PAGE: Arterial Pressure
- Page 2: Hypertension Categories
- Page 3: Causes of Hypertension
- Page 4: Antihypertensive Drugs
Arterial Pressure
Arterial blood pressure is generated by the left ventricle ejecting blood into the systemic vasculature, which acts as a resistance to cardiac output. With each ejection of blood during ventricular systole, the aortic blood volume increases, which stretches the wall of the aorta and increases aortic pressure. As the heart relaxes (ventricular diastole), blood flows from the aorta into distributing arteries that transport the blood to the various organs. Within the organs, the arterial vasculature undergoes extensive branching and the vessel diameters decrease. The smaller arteries and arterioles serve as the chief resistance vessels, and through changes in their diameter, regulate systemic vascular resistance and organ blood flow.
In the aorta and arterial vessels, the arterial pressure is pulsatile, but by the time the blood reaches the capillaries, the pulsatility has been removed by vascular dampening. In hemodynamic terms, it is the mean arterial pressure (MAP) that drives organ blood flow. MAP can be described hemodynamically as the product of cardiac output (CO) and systemic vascular resistance (SVR), plus the central venous pressure (CVP).
Equation 1: MAP = (CO x SVR) + CVP
Based on this equation, increases in CO, SVR or CVP can lead to increases in MAP, with changes in CO and SVR having a quantitatively dominant effect in different hypertensive conditions.
While MAP is an important hemodynamic parameter and is required for calculating SVR, it is not measured in clinical practice unless a person's arterial pressure is being monitored with an indwelling catheter. The most common method for measuring arterial pressure is by use of a sphygmomanometer, which gives systolic and diastolic pressure values in mmHg. The systolic pressure is the peak arterial pressure that occurs during ventricular systole, whereas the diastolic pressure is the minimal aortic pressure just before the ventricle ejects blood into the aortic. At normal heart rates, MAP can be estimated from the systolic (Psys) and diastolic (Pdias) pressure values by the following equation:
Equation 2: MAP = 1/3 (Psys - Pdias) + Pdias
This equation is useful for estimating MAP from systolic and diastolic pressure values; however, this equation does not describe the hemodynamic variables that determine MAP. The hemodynamic variables that determine MAP are found in Equation 1.
Hypertension Categories
Several leading physician organizations, including the American Heart Association and the American College of Cardiology, published new guidelines in November 2017 for defining and treating hypertension. Based on large-scale clinical studies, the following definitions are now applied to adults:
| Category | Systolic | Diastolic (mmHg) | |
| Normal | < 120 | and | < 80 |
| Elevated | 120 – 129 | and | < 80 |
| Hypertension | |||
| Stage 1 | 130 – 139 | or | 80 – 89 |
| Stage 2 | ≥ 140 | or | ≥ 9 |
It is important to note that a hypertensive state is defined as an abnormal elevation of either systolic or diastolic pressure. In past years, the diastolic value was emphasized in determining whether a person was hypertensive. However, elevations in systolic pressure ("systolic hypertension") are also associated with increased incidence of coronary and cerebrovascular disease (e.g., stroke). Therefore, we now recognize that both systolic and diastolic pressure values are important for assessing clinical states of hypertension.
Causes of Hypertension
There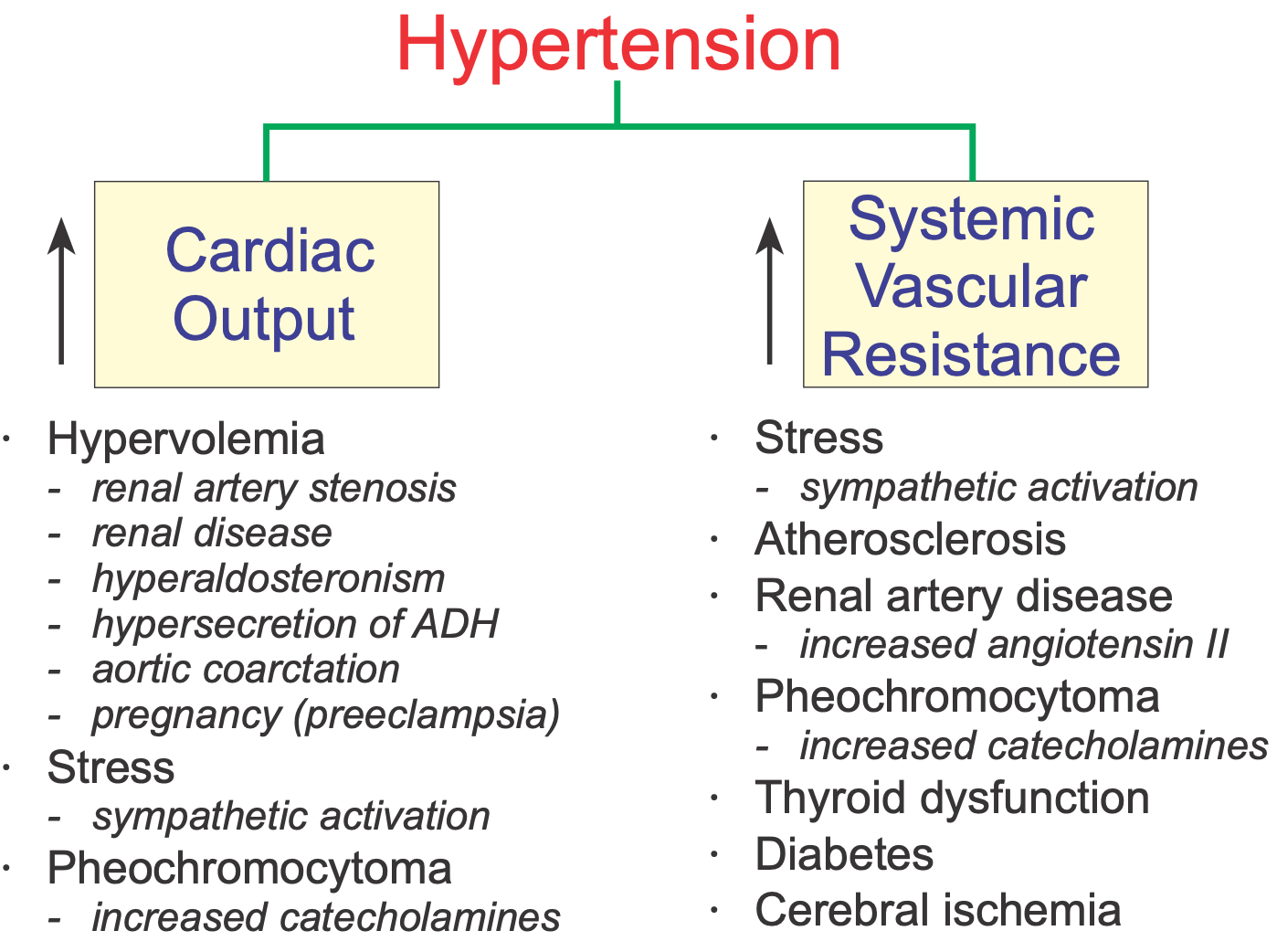 are two basic types of hypertension: primary (essential) hypertension and secondary hypertension. The vast majority of patients (90-95%) have essential hypertension, which is a form with no identifiable underlying cause. This form of hypertension is commonly treated with drugs in addition to lifestyle changes (e.g., exercise, proper nutrition, weight reduction, stress reduction).
are two basic types of hypertension: primary (essential) hypertension and secondary hypertension. The vast majority of patients (90-95%) have essential hypertension, which is a form with no identifiable underlying cause. This form of hypertension is commonly treated with drugs in addition to lifestyle changes (e.g., exercise, proper nutrition, weight reduction, stress reduction).
A smaller number of patients (5-10%) have secondary hypertension that is caused by an identifiable underlying condition such as renal artery disease, thyroid disease, primary hyperaldosteronism, pregnancy, etc.
As previously described, hypertension results from increased cardiac output, increased systemic vascular resistance, or both. The figure summarizes conditions that can increase either cardiac output or systemic vascular resistance.
Some causes of secondary hypertension are listed below:
- Renal artery stenosis
- Chronic renal disease
- Primary hyperaldosteronism
- Stress
- Sleep apnea
- Hyper- or hypothyroidism
- Pheochromocytoma
- Preeclampsia
- Aortic coarctation
Renal artery stenosis (renovascular disease)
Renal artery disease can cause narrowing of the vessel lumen (stenosis). The reduced lumen diameter increases the pressure drop along the length of the diseased renal artery, which reduces the pressure at the afferent arteriole in the kidney. Reduced arteriolar pressure and reduced renal perfusion stimulate renin release by the kidney, which leads to increased circulating angiotensin II (AII) and aldosterone. These hormones increase blood volume by enhancing renal reabsorption of sodium and water. This increases blood volume, which augments cardiac output by the Frank-Starling mechanism. Increased AII directly produces systemic vasoconstriction (increased systemic vascular resistance) and enhances sympathetic activity, which indirectly causes further vasoconstriction and cardiac stimulation. Chronic elevation of AII promotes cardiac and vascular hypertrophy. Therefore, hypertension caused by renal artery stenosis results from both an increase in systemic vascular resistance and an increase in cardiac output.
Chronic renal disease
Many pathologic processes (e.g., diabetic nephropathy, glomerulonephritis) can damage nephrons in the kidney. When this occurs, the kidney cannot excrete normal amounts of sodium, which leads to sodium and water retention, increased blood volume, and increased cardiac output by the Frank-Starling mechanism. Renal disease may also result in increased release of renin, leading to a renin-dependent form of hypertension. The elevation in arterial pressure secondary to renal disease can be viewed as an attempt by the kidney to increase renal perfusion and restore glomerular filtration.
Primary hyperaldosteronism
Increased secretion of aldosterone resulting from adrenal adenoma or adrenal hyperplasia is a form of primary hyperaldosteronism. In contrast, secondary hyperaldosteronism results from elevated renin and angiotensin II. Increased circulating aldosterone causes renal retention of sodium and water, therefore blood volume and arterial pressure increase. Plasma renin levels are usually decreased in primary hyperaldosteronism as the body attempts to suppress the renin-angiotensin system; there is also hypokalemia associated with the high levels of aldosterone.
Stress
Emotional stress leads to activation of the sympathetic nervous system, which causes increased release of norepinephrine from sympathetic nerves in the heart and blood vessels, leading to increased cardiac output and increased systemic vascular resistance. Additionally, stress stimulates the adrenal medulla to secrete more catecholamines (epinephrine and norepinephrine). Activation of the sympathetic nervous system increases circulating angiotensin II, aldosterone, and vasopressin, which increases systemic vascular resistance and blood volume. Prolonged elevation of angiotensin II and catecholamines can lead to cardiac and vascular hypertrophy, both of which can contribute to a sustained increase in blood pressure.
Sleep Apnea
Sleep apnea is a disorder in which people repeatedly stop breathing for short periods of time (10-30 seconds) during their sleep. This condition is often associated with obesity, although it can have other causes, such as airway obstruction or disorders of the central nervous system. These individuals have a higher incidence of hypertension. The mechanism of hypertension may be related to sympathetic activation and hormonal changes associated with repeated periods of apnea-induced hypoxia and hypercapnia, and from stress associated with the loss of sleep.
Hyper- or hypothyroidism
Excessive thyroid hormone induces systemic vasoconstriction, increased blood volume, and increased cardiac activity, all of which can lead to hypertension. It is less clear why some patients with hypothyroidism develop hypertension, but it may be related to decreased tissue metabolism, which reduces the production and release of vasodilator metabolites and causes vasoconstriction and increased systemic vascular resistance.
Pheochromocytoma
Catecholamine secreting tumors in the adrenal medulla can lead to very high levels of circulating catecholamines (both epinephrine and norepinephrine). This leads to alpha-adrenoceptor mediated systemic vasoconstriction and beta-adrenoceptor mediated cardiac stimulation, both of which contribute to significant elevations in arterial pressure. Despite the elevation in arterial pressure, which would ordinarily activate a baroreflex-induced bradycardia, tachycardia occurs because of the direct effects of the catecholamines on the heart and vasculature. Excessive beta-adrenoceptor stimulation in the heart often leads to arrhythmias. Pheochromocytoma is diagnosed by measuring plasma or urine catecholamine levels and their metabolites (vanillylmandelic acid and metanephrine).
Preeclampsia
This is a condition that sometimes develops during the third trimester of pregnancy that causes hypertension due to increased blood volume and tachycardia. The former increases cardiac output by the Frank-Starling mechanism.
Aortic coarctation
Coarctation, or narrowing of the aorta (typically just distal to the left subclavian artery), is a congenital defect that obstructs aortic outflow, leading to elevated pressures proximal to the coarctation (i.e., elevated arterial pressures in the head and arms). Distal pressures, however, are not necessarily reduced as expected from the hemodynamics associated with a stenosis. The reason for this is that reduced renal blood flow leads to an increase in the release of renin and an activation of the renin-angiotensin-aldosterone system. This elevates blood volume and arterial pressure. Although the aortic arch and carotid sinus baroreceptors are exposed to higher-than-normal pressures because they are proximal to the coarctation, the baroreceptor reflex is blunted because of structural changes in the walls of vessels where the baroreceptors are located. Also, baroreceptors become desensitized to chronic elevation in pressure and become "reset" to the higher pressure.
Go to Next Page
Antihypertensive Drugs
Revised 02/04/2023
 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)