Angiotensin Converting Enzyme (ACE) Inhibitors
General Pharmacology
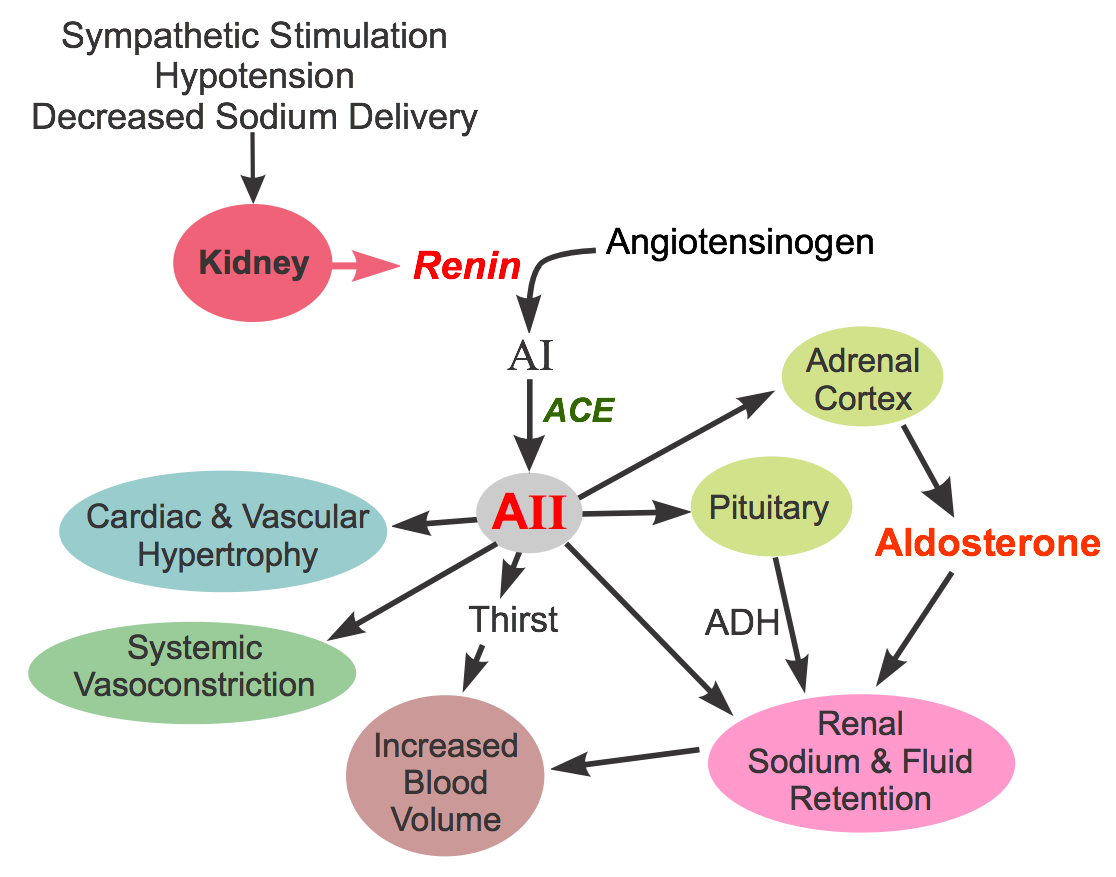 ACE inhibitors produce vasodilation by inhibiting the formation of angiotensin II. This vasoconstrictor is formed by the proteolytic action of renin (released by the kidneys) acting on circulating angiotensinogen to form angiotensin I. Angiotensin I is then converted to angiotensin II by angiotensin converting enzyme (ACE).
ACE inhibitors produce vasodilation by inhibiting the formation of angiotensin II. This vasoconstrictor is formed by the proteolytic action of renin (released by the kidneys) acting on circulating angiotensinogen to form angiotensin I. Angiotensin I is then converted to angiotensin II by angiotensin converting enzyme (ACE).
ACE also breaks down bradykinin (a vasodilator substance). Therefore, ACE inhibitors, by blocking the breakdown of bradykinin, increase bradykinin levels, which can contribute to the vasodilator action of ACE inhibitors. The increase in bradykinin is also believed to be responsible for a troublesome side effect of ACE inhibitors, a dry cough.
Angiotensin II constricts arteries and veins by binding to AT1 receptors on the smooth muscle, which are coupled to a Gq-protein and the IP3 signal transduction pathway. Angiotensin II also facilitates the release of norepinephrine from sympathetic adrenergic nerves and inhibits norepinephrine reuptake by these nerves. This action of angiotensin II augments sympathetic activity on the heart and blood vessels, promoting cardiac stimulation and vasoconstriction. Angiotensin II stimulates the adrenal cortex to release aldosterone, which acts on the kidneys to increase sodium and water reabsorption, leading to increased blood volume and arterial pressure. By stimulating pituitary release of antidiuretic hormone (ADH; vasopressin), water renal reabsorption is increased, which increases blood volume and arterial pressure. ADH can also directly constrict blood vessels.
ACE inhibitors have the following actions: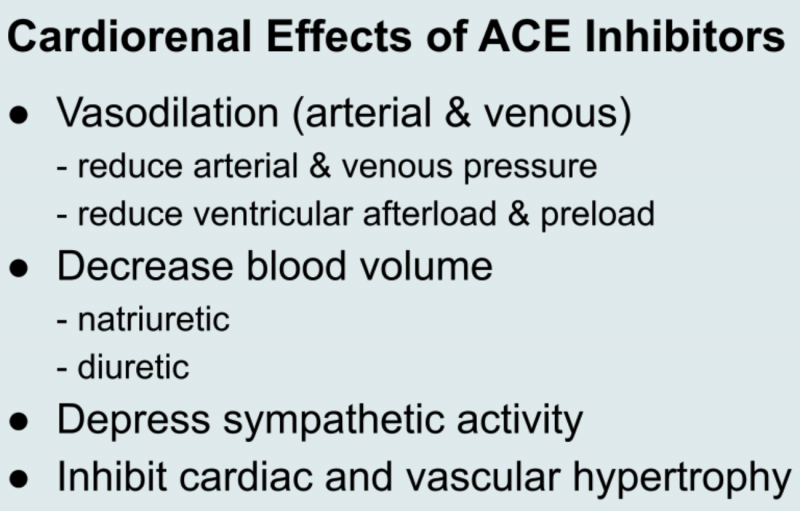
- Dilate arteries and veins by blocking angiotensin II formation and inhibiting bradykinin metabolism. This vasodilation reduces arterial pressure, preload and afterload on the heart.
- Down regulate sympathetic adrenergic activity by blocking the facilitating effects of angiotensin II on sympathetic nerve release and reuptake of norepinephrine.
- Promote renal excretion of sodium and water (natriuretic and diuretic effects) by blocking the effects of angiotensin II in the kidney, blocking angiotensin II stimulation of aldosterone secretion, and by blocking angiotensin II stimulated ADH release. These actions blood volume, venous pressure and arterial pressure.
- Inhibit cardiac and vascular remodeling associated with chronic hypertension, heart failure, and myocardial infarction.
Elevated plasma renin is not required for the actions of ACE inhibitors, although ACE inhibitors are more efficacious when circulating levels of renin are elevated. We know that the renin-angiotensin system is found in many tissues, including the heart, brain, vascular and renal tissues. Therefore, ACE inhibitors may act at these sites besides blocking the conversion of angiotensin in the circulating plasma.
Therapeutic Uses
Hypertension
ACE inhibitors are considered "first-line therapy" in the treatment of stage 1 hypertension. They may also be used in hypertension caused by renal artery stenosis, which causes renin-dependent hypertension owing to the increased release of renin by the kidneys. Reducing angiotensin II formation leads to arterial and venous dilation, which reduces arterial and venous pressures. By reducing the effects of angiotensin II on the kidney, ACE inhibitors cause natriuresis and diuresis, which decreases blood volume and cardiac output, lowering arterial pressure.
African Americans do not respond as well as other races to monotherapy with ACE inhibitors or angiotensin receptor blockers (ARBs); however, differences in blood pressure lowering efficacy are eliminated with adequate diuretic dosing. Therefore, current recommendations are that ACE inhibitors and ARBs are appropriate for African Americans, but not as monotherapy. A diuretic or calcium-channel blocker should be used with an ACE inhibitor or ARB to achieve the target reduction in blood pressure in these patient populations.
Heart Failure
ACE inhibitors have proven to be very effective in the treatment of heart failure caused by systolic dysfunction (i.e., heart failure with reduced ejection fraction; HFrEF). Beneficial effects of ACE inhibition in HFrEF include:
- Reduced afterload, which enhances ventricular stroke volume and improves ejection fraction.
- Reduced preload, which decreases pulmonary and systemic congestion and edema.
- Reduced sympathetic activation, which is deleterious in chronic heart failure.
- Improving the oxygen supply/demand ratio, primarily by decreasing demand through the reductions in afterload and preload.
- Prevents angiotensin II from triggering deleterious cardiac remodeling.
Note that ACE inhibitors are often used with a diuretic in treating hypertension and heart failure.
Myocardial infarction
Finally, ACE inhibitors are effective in patients following myocardial infarction because they help to reduce deleterious remodeling that occurs post-infarction.
Specific Drugs
The first ACE inhibitor marketed, captopril, is still in widespread use today, although its short half-life requires dosing 2-3 times per day. Newer ACE inhibitors differ from captopril in terms of pharmacokinetics (e.g., longer half-life) and metabolism; however, all ACE inhibitors have similar overall effects on blocking the formation of angiotensin II. Many of the drugs are converted to a more active form after absorption. The following is a list of ACE inhibitors available for clinical use:
- benazepril
- captopril
- cilazapril
- enalapril (prodrug that forms enalaprilat)
- enalaprilat (I.V. only)
- fosinopril
- lisinopril
- moexipril
- perindopril
- quinapril
- ramipril
- tradolapril
Note that each of the ACE inhibitors named above ends with "pril."
Side Effects and Contraindications
As a drug class, ACE inhibitors have a relatively low incidence of side effects and are well-tolerated. A common, annoying side effect of ACE inhibitors is a dry cough, appearing in about 10% of patients. It appears to be related to the elevation in bradykinin. Hypotension can also be a problem, especially in heart failure patients. Angioedema (life-threatening airway swelling and obstruction; 0.1-0.2% of patients) and hyperkalemia (occurs because aldosterone formation is reduced) are also adverse effects of ACE inhibition. The incidence of angioedema is 2 to 4-times higher in African Americans compared to Caucasians. ACE inhibitors are contraindicated in pregnancy.
Hypertensive patients caused by bilateral renal artery stenosis may experience renal failure if ACE inhibitors are administered. The reason is that elevated circulating and intrarenal angiotensin II in this condition constricts the efferent arteriole more than the afferent arteriole within the kidney, which helps to maintain glomerular capillary pressure and filtration. Removing this constriction by blocking circulating and intrarenal angiotensin II formation can cause an abrupt fall in glomerular filtration rate. This is not generally a concern with unilateral renal artery stenosis because the unaffected kidney can usually maintain sufficient filtration after ACE inhibition; however, with bilateral renal artery stenosis, it is especially important to ensure that renal function is not compromised.
Revised 12/05/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)