Alpha-Adrenoceptor Agonists (α-agonists)
General Pharmacology
Most alpha-adrenoceptor agonists (α-agonists) that are used clinically bind to α-receptors on vascular smooth muscle and induce smooth contraction and vasoconstriction, thus mimicking the effects of sympathetic adrenergic nerve activation to the blood vessels. Some α-agonists bind to prejunctional receptors on sympathetic nerves, which inhibits norepinephrine release both peripherally and centrally in the brain.
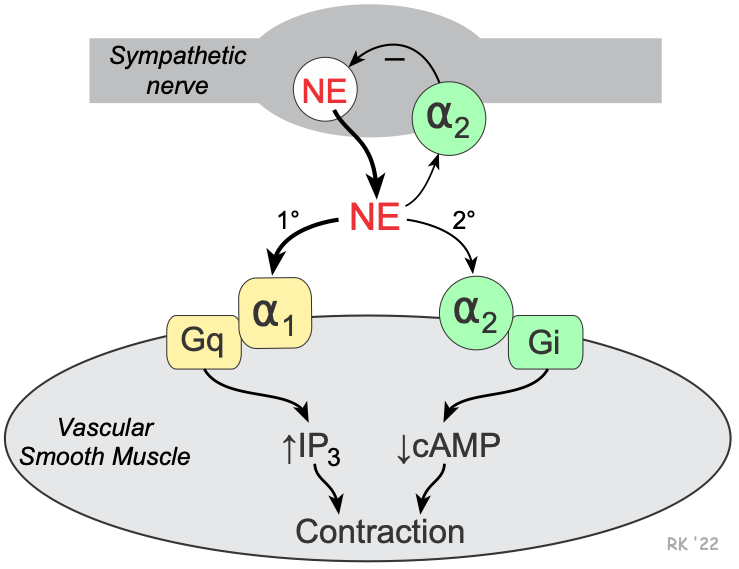 Vascular smooth muscle has two types of alpha-adrenoceptors — alpha1 (α1) and alpha2 (α2). The α1-adrenoceptors are the predominant α-receptors on vascular smooth muscle. These receptors are linked to Gq-proteins that activate smooth muscle contraction through the IP3 signal transduction pathway and Rho-kinase pathway. Depending on the tissue and type of vessel, there are also α2-adrenoceptors found on the smooth muscle. These receptors are linked to Gi-proteins, and binding of a α2-agonist to these receptors decreases intracellular cAMP, which causes smooth muscle contraction. There are also α2-adrenoceptors located on the sympathetic nerve terminals that inhibit the release of norepinephrine and therefore act as a feedback mechanism for modulating the release of norepinephrine. Therefore, an α2-agonist inhibits norepinephrine release from sympathetic nerves.
Vascular smooth muscle has two types of alpha-adrenoceptors — alpha1 (α1) and alpha2 (α2). The α1-adrenoceptors are the predominant α-receptors on vascular smooth muscle. These receptors are linked to Gq-proteins that activate smooth muscle contraction through the IP3 signal transduction pathway and Rho-kinase pathway. Depending on the tissue and type of vessel, there are also α2-adrenoceptors found on the smooth muscle. These receptors are linked to Gi-proteins, and binding of a α2-agonist to these receptors decreases intracellular cAMP, which causes smooth muscle contraction. There are also α2-adrenoceptors located on the sympathetic nerve terminals that inhibit the release of norepinephrine and therefore act as a feedback mechanism for modulating the release of norepinephrine. Therefore, an α2-agonist inhibits norepinephrine release from sympathetic nerves.
Alpha-agonists constrict both arteries and veins; however, the vasoconstrictor effect is more pronounced in the arterial resistance vessels. Constriction of the resistance vessels (small arteries and arterioles) increases systemic vascular resistance, whereas constriction of venous capacitance vessels increases venous pressure.
Specific Drugs and Therapeutic Uses
Alpha-agonists used therapeutically are relatively selective or non-selective for α1 or α2-adrenoceptors. Besides the drugs listed below, there are sympathomimetic drugs that have α-agonist and β-adrenoceptor agonist properties. These drugs include the naturally occurring catecholamines, dopamine, epinephrine and norepinephrine.
Alpha1-adrenoceptor agonists (systemic vasoconstrictors)
- midodrine (prodrug converted to desglymidodrine)
- phenylephrine and related compounds
- Phenylephrine (I.V. form) is used as a pressor agent in treating hypotension and shock. Midodrine (oral form) is used in patients with autonomic insufficiency and symptomatic postural hypotension.
- Oxymetazoline, tetrahydrozoline, xylometazoline and some preparations of phenylephrine are used as nasal decongestants primarily because of their α1-mediated vasoconstrictor properties.
Alpha2-adrenoceptor agonists (centrally acting vasodilators; Click here for details)
- clonidine
- guanabenz
- guanfacine
- methyldopa
Side Effects and Contraindications — α1-agonists
Alpha1-agonists can cause headache, reflex bradycardia, excitability, and restlessness. Because alpha1-agonists produce systemic vasoconstriction, the work, and oxygen requirements of the heart increase. If the coronary circulation is impaired, as in patients with coronary artery disease, the decrease in myocardial oxygen supply/demand ratio can precipitate angina. Preparations used as nasal decongestants can cause a rebound effect (increased congestion) after a few days of use.
Revised 01/14/2024

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)