Thrombolytic (Fibrinolytic) Drugs
Thrombolytic drugs are used to dissolve (lyse) blood clots (thrombi). Blood clots can occur in any vascular bed; however, when they occur in coronary, cerebral or pulmonary vessels, they can be immediately life-threatening. Coronary thrombi cause myocardial infarction, cerebrovascular thrombi produce strokes, and pulmonary thrombi can lead to respiratory and cardiac failure. Therefore, rapid diagnosis and treatment of blood clots is important.
Mechanisms of Thrombolysis
Thrombolytic drugs dissolve blood clots by activating plasminogen, which forms a cleaved product called plasmin. Plasmin is a proteolytic enzyme that breaks cross-links between fibrin molecules, which provide the structural integrity of blood clots. Because of these actions, thrombolytic drugs are also called "plasminogen activators" and "fibrinolytic drugs."
There are three major classes of fibrinolytic drugs: tissue plasminogen activator (tPA), streptokinase (SK), and urokinase (UK). While drugs in these three classes all effectively dissolve blood clots, they differ in their mechanisms, which alter their selectivity for fibrin clots.
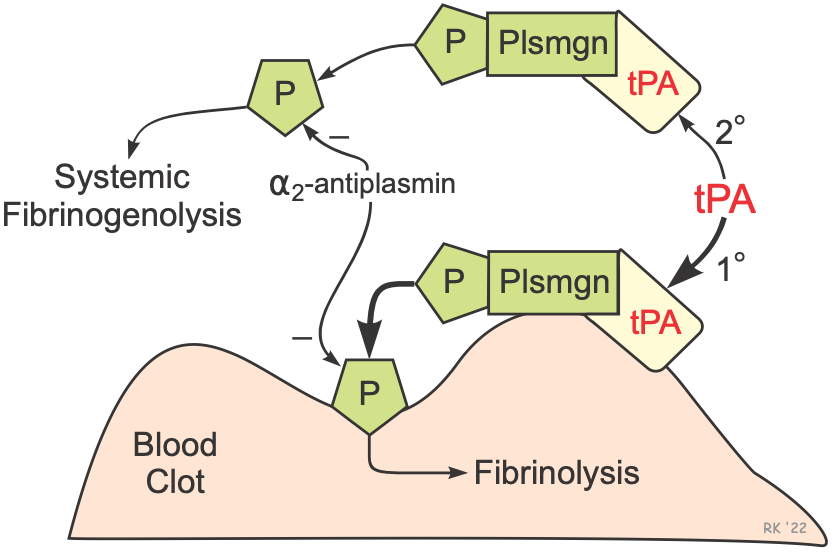
The figure illustrates the fibrinolytic mechanisms for tPA. Derivatives of tPA are the most used thrombolytic drugs because of their relative selectivity for activating fibrin-bound plasminogen. Tissue plasminogen activator produces clot lysis through the following sequence:
- tPA binds to fibrin on the surface of the clot
- Activates fibrin-bound plasminogen
- Plasmin is cleaved from the plasminogen associated with the fibrin
- Fibrin molecules are broken apart by the plasmin and the clot dissolves
Plasmin is a protease that can break apart fibrin molecules, dissolving the clot. However, it is important to note that plasmin also breaks down other circulating proteins, including fibrinogen. But because of the relative fibrin specificity of tPA, clot dissolution occurs with a less breakdown of circulating fibrinogen than occurs with SK and UK. Although tPA is relatively selective for clot-bound plasminogen, it still activates circulating plasminogen and releases plasmin, which can lead to the breakdown of circulating fibrinogen and cause an unwanted systemic fibrinolytic state. Normally, circulating α2-antiplasmin inactivates plasmin, but therapeutic doses of tPA (and SK) lead to sufficient plasmin formation to overwhelm the limited circulating concentrations α2-antiplasmin. In summary, although tPA is relatively selective for clot-associated fibrin, it can produce systemic lytic state and undesirable bleeding.
SK is not a protease and has no enzymatic activity; however, it forms a complex with plasminogen that releases plasmin. Unlike tPA, it does not bind preferentially to clot-associated fibrin and therefore binds equally to circulating and non-circulating plasminogen. Therefore, SK produces significant fibrinogenolysis along with clot fibrinolysis. Because SK is derived from streptococci, patients who have had recent streptococci infections can require significantly higher doses of SK to produce thrombolysis.
It is important to note that the efficacy of thrombolytic drugs depends on the age of the clot. Older clots have more fibrin cross-linking and are more compacted; therefore, older clots are more difficult to dissolve. For treating acute myocardial infarction, the thrombolytic drugs should ideally be given within the first 2 hours. Beyond that time, the efficacy diminishes, and higher doses are required to achieve desired lysis.
Therapeutic Indications for Thrombolytic Drugs
Thrombolytic agents are used for the following therapeutic indications:
- Acute myocardial infarction (ST-elevated; STEMI)
- Acute pulmonary embolism
- Acute ischemic stroke (non-hemorrhagic)
- Acute limb ischemia (arterial thrombosis)
- Deep vein thrombosis (DVT)
Specific Thrombolytic Drugs
Tissue Plasminogen Activators
This family of thrombolytic drugs is used for all the above indications.
- Alteplase (Activase®; rtPA) is a recombinant form of human tPA. It has a short half-life (~5 min) and therefore is usually administered as an intravenous bolus followed by an infusion.
- Retaplase (Retavase®) is a genetically engineered, smaller derivative of recombinant tPA that has increased potency and is faster acting than rtPA. Having a longer half-life than rtPA, it is often administered as IV bolus injections.
- Tenecteplase (TNK-tPA) has a longer half-life and greater binding affinity for fibrin than rtPA. Because of its longer half-life, it can be administered by IV bolus.
Streptokinase (SK) and Urokinase (UK)
The use of these drugs has been superseded by tPA-compounds because of issues related to specificity of action, systemic fibrinolysis, and ease of administration. Neither SK nor UK are available for use in the U.S.
Natural streptokinase (SK) is isolated and purified from streptococci bacteria. Its lack of fibrin specificity makes it a less desirable thrombolytic drug than tPA compounds because it produces more fibrinogenolysis. SK is antigenic because it is derived from streptococci bacteria and, therefore, neutralizing antibodies can decrease its effectiveness.
Anistreplase (Eminase®) is a complex of SK and plasminogen and therefore is antigenic, like SK alone. It has more fibrin specificity and has a longer activity than natural SK; however, it causes considerable fibrinogenolysis.
Urokinase (Abbokinase®; UK) is sometimes referred to as urinary-type plasminogen activator (uPA) because it is formed by the kidneys and is found in urine. It has limited clinical use because, like SK, it produces considerable fibrinogenolysis, although it is non-antigenic.
Adverse Effects and Contraindications
A common adverse effect of all the thrombolytic drugs is bleeding complications related to systemic fibrinogenolysis and lysis of normal hemostatic plugs. The bleeding is often noted at a catheterization site, although gastrointestinal and cerebral hemorrhages may occur. Intracranial bleeding is a significant concern (5-7%) in using I.V. rtPA for acute ischemic stroke. Therefore, patients who have experienced trauma injury or who have a history of cerebral hemorrhagic stroke are not usually administered thrombolytics. Re-thrombosis can occur following thrombolysis, and therefore anticoagulants such as heparin are typically co-administered and continued after thrombolytic therapy.
Revised 11/30/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)