Beta-Adrenoceptor Antagonists (Beta-Blockers)
General Pharmacology
Beta-blockers are drugs that bind to beta-adrenoceptors and block the binding of norepinephrine and epinephrine to these receptors. This inhibits normal sympathetic effects that act through these receptors. Therefore, beta-blockers are sympatholytic drugs. Some beta-blockers, when they bind to the beta-adrenoceptor, partially activate the receptor while preventing norepinephrine from binding to the receptor. These partial agonists therefore provide some "background" of sympathetic activity while preventing normal and enhanced sympathetic activity. Partial agonist beta-blockers possess intrinsic sympathomimetic activity (ISA). Some beta-blockers also possess membrane stabilizing activity (MSA), which is similar to the membrane stabilizing activity of sodium-channels blockers (Class I antiarrhythmics).
The first generation of beta-blockers are non-selective, meaning that they block both beta-1 (β1) and beta-2 (β2) adrenoceptors. Second generation beta-blockers are more cardioselective in that they are relatively selective for β1 adrenoceptors. Note that this relative selectivity can be lost at higher drug doses. Finally, third generation beta-blockers are drugs that also possess vasodilator actions by blocking vascular alpha-adrenoceptors.
Heart
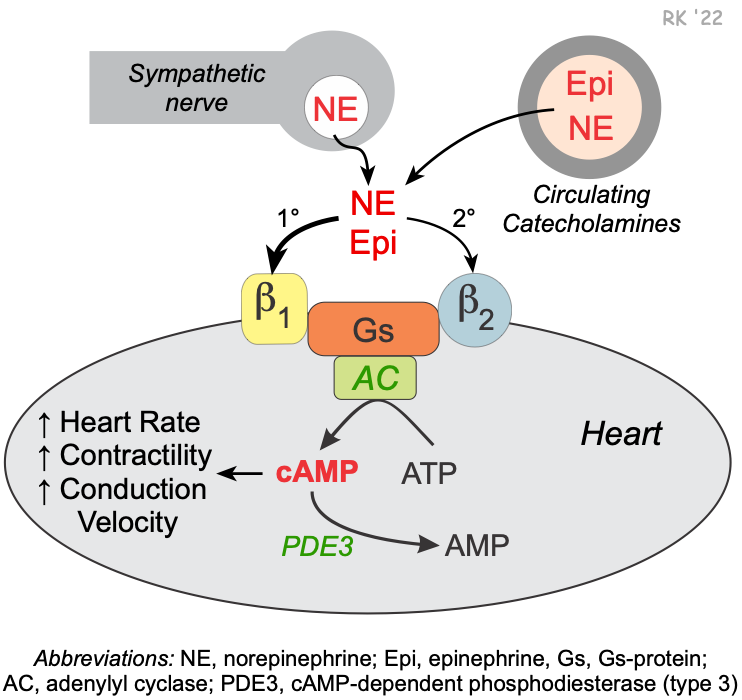 Beta-blockers bind to beta-adrenoceptors in cardiac nodal tissue, the conducting system, and contracting myocytes. The heart has both β1 and β2 adrenoceptors, although the predominant receptor type in number and function is β1. These receptors primarily bind norepinephrine that is released from sympathetic adrenergic nerves. Additionally, they bind to norepinephrine and epinephrine that circulate in the blood. Beta-blockers prevent the normal ligand (norepinephrine or epinephrine) from binding to the beta-adrenoceptor by competing for the binding site.
Beta-blockers bind to beta-adrenoceptors in cardiac nodal tissue, the conducting system, and contracting myocytes. The heart has both β1 and β2 adrenoceptors, although the predominant receptor type in number and function is β1. These receptors primarily bind norepinephrine that is released from sympathetic adrenergic nerves. Additionally, they bind to norepinephrine and epinephrine that circulate in the blood. Beta-blockers prevent the normal ligand (norepinephrine or epinephrine) from binding to the beta-adrenoceptor by competing for the binding site.
Beta-adrenoceptors are coupled to a Gs-proteins, which activate adenylyl cyclase to form cAMP from ATP. Increased cAMP activates a cAMP-dependent protein kinase (PK-A) that phosphorylates L-type calcium channels, which causes increased calcium entry into the cell. Increased calcium entry during action potentials causes enhanced release of calcium by the sarcoplasmic reticulum in the heart; these actions increase inotropy (contractility). Gs-protein activation also increases heart rate (chronotropy) by increasing phase 4 pacemaker currents in the sinoatrial node. PK-A phosphorylates sites on the sarcoplasmic reticulum, which leads to enhanced release of calcium through the ryanodine receptors (ryanodine-sensitive, calcium-release channels) associated with the sarcoplasmic reticulum. This provides more calcium for binding the troponin-C, which enhances inotropy. Finally, PK-A can phosphorylate myosin light chains, which may contribute to the positive inotropic effect of beta-adrenoceptor stimulation.
Because there is some level of sympathetic tone on the heart, beta-blockers can reduce sympathetic influences that normally stimulate chronotropy (heart rate), inotropy (contractility), dromotropy (electrical conduction) and lusitropy (relaxation). Therefore, beta-blockers cause decreases in heart rate, contractility, conduction velocity, and relaxation rate. These drugs have an even greater effect when there is elevated sympathetic activity.
Blood vessels
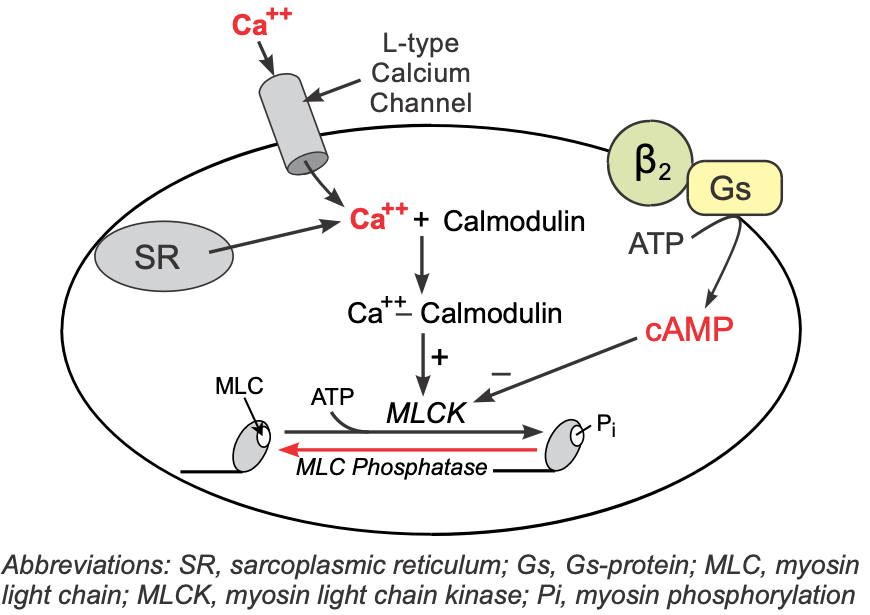 Vascular smooth muscle has β2-adrenoceptors that are normally activated by norepinephrine released by sympathetic adrenergic nerves or by circulating epinephrine. These receptors, like those in the heart, are coupled to a Gs-protein that stimulates the formation of cAMP. Although increased cAMP enhances cardiac myocyte contraction (see above), in vascular smooth muscle an increase in cAMP leads to smooth muscle relaxation. This is because cAMP inhibits myosin light chain kinase that phosphorylates smooth muscle myosin. Therefore, increases in intracellular cAMP caused by β2-agonists inhibit myosin light chain kinase, producing less contractile force (i.e., promoting relaxation).
Vascular smooth muscle has β2-adrenoceptors that are normally activated by norepinephrine released by sympathetic adrenergic nerves or by circulating epinephrine. These receptors, like those in the heart, are coupled to a Gs-protein that stimulates the formation of cAMP. Although increased cAMP enhances cardiac myocyte contraction (see above), in vascular smooth muscle an increase in cAMP leads to smooth muscle relaxation. This is because cAMP inhibits myosin light chain kinase that phosphorylates smooth muscle myosin. Therefore, increases in intracellular cAMP caused by β2-agonists inhibit myosin light chain kinase, producing less contractile force (i.e., promoting relaxation).
Compared to their effects in the heart, beta-blockers have relatively little direct vascular effect because β2-adrenoceptors have only a small modulator role on basal vascular tone. Blockade of β2-adrenoceptors is associated with a small amount of vasoconstriction in many vascular beds. This occurs because beta-blockers remove a small β2-adrenoceptor vasodilator influence (e.g., originating from circulating epinephrine) that is normally opposing the more dominant alpha-adrenoceptor mediated vasoconstrictor influence originating from sympathetic tone.
Therapeutic Indications
Beta-Blockers
Cardiac Effects
- Decrease contractility
(- inotropy) - Decrease relaxation rate
(- lusitropy) - Decrease heart rate
(- chronotropy) - Decrease conduction velocity
(- dromotropy)
Vascular Effects
- Smooth muscle contraction
(mild vasoconstriction)
Beta-blockers are used for treating hypertension, angina, myocardial infarction, arrhythmias, and heart failure.
Hypertension
Beta-blockers decrease arterial blood pressure by reducing cardiac output. Many causes of hypertension are associated with an increase in blood volume and cardiac output. Therefore, reducing cardiac output by beta-blockade can be an effective treatment for hypertension, especially when used with a diuretic. Acute treatment with a beta-blocker is not very effective in reducing arterial pressure because of a compensatory increase in systemic vascular resistance produced by baroreceptor reflexes. Chronic treatment with beta-blockers lowers arterial pressure more than acute treatment, possibly because of reduced release of renin by the kidneys (the release of which is partly regulated by β1-adrenoceptors in the kidney). Decreasing circulating plasma renin leads to a decrease in angiotensin II and aldosterone, which enhances renal loss of sodium and water and further diminishes arterial pressure. Hypertension in some patients is caused by emotional stress, which causes enhanced sympathetic activity. Beta-blockers can be very effective in these patients.
Therapeutic Use of
Beta-Blockers
- Hypertension
- Angina
- Myocardial infarction
- Arrhythmias
- Heart failure
Beta-blockers are used in the preoperative management of hypertension caused by a pheochromocytoma, which results in elevated circulating catecholamines. When used for this condition, the blood pressure is first controlled using an alpha-blocker such as phenoxybenzamine, and then a beta-blocker can be carefully administered to reduce the excessive cardiac stimulation by the catecholamines. It is important that a beta-blocker is administered only after blockade of vascular alpha-adrenoceptors so that a hypertensive crisis does not occur because of unopposed alpha-adrenoceptor stimulation.
Angina and myocardial infarction
The antianginal effects of beta-blockers are attributed to their cardiodepressant and hypotensive actions. By reducing heart rate, contractility, and arterial pressure, beta-blockers reduce the work of the heart and the oxygen demand of the heart. Reducing oxygen demand improves the oxygen supply/demand ratio, which can relieve a patient of anginal pain that is caused by a coronary artery disease. Furthermore, beta-blockers are frequently used in treating myocardial infarction because they have been shown to decrease mortality. Their benefit is derived not only from improving the oxygen supply/demand ratio and reducing arrhythmias, but also from their ability to inhibit subsequent cardiac remodeling.
Arrhythmias
The antiarrhythmic properties of beta-blockers (Class II antiarrhythmic) are related to their ability to inhibit sympathetic influences on cardiac electrical activity. Sympathetic nerves increase sinoatrial node automaticity by increasing the pacemaker currents, which increases sinus rate. Sympathetic activation also increases conduction velocity (particularly at the atrioventricular node), and stimulates aberrant pacemaker activity (ectopic foci). These sympathetic influences are mediated primarily through β1-adrenoceptors. Therefore, beta-blockers can attenuate these sympathetic effects and decrease sinus rate, decrease conduction velocity (which can block reentry mechanisms), and inhibit aberrant pacemaker activity. Beta-blockers also affect non-pacemaker action potentials by increasing action potential duration and the effective refractory period. This effect can play a major role in blocking arrhythmias caused by reentry.
Heart failure
Most patients in heart failure have a form that is called systolic dysfunction (HFrEF), in which the contractile function of the heart is depressed (loss of inotropy) and ejection fraction is. Although it seems counterintuitive that cardioinhibitory drugs such as beta-blockers would be used in cases of systolic dysfunction, clinical studies have shown conclusively that some specific beta-blockers improve cardiac function and reduce mortality. Additionally, they reduce the deleterious cardiac remodeling that occurs in chronic heart failure. Although the exact mechanism by which beta-blockers confer their benefit to heart failure patients is poorly understood, it may be related to the blockade of excessive, chronic sympathetic stimulation of the heart. This is known to be harmful to the failing heart. Note in the table of drugs that, based upon clinical trials, only three beta-blockers are FDA approved for heart failure — carvedilol, metoprolol and bisoprolol.
Different Classes of Beta-Blockers and Specific Drugs
Beta-blockers that are used clinically can be divided into two classes: 1) non-selective blockers (block both β1 and β2 receptors), or 2) relatively selective β1 blockers ("cardioselective" beta-blockers). Some beta-blockers have additional mechanisms besides beta-blockade that contribute to their unique pharmacologic profile. The two classes of beta-blockers along with specific compounds are listed in the following table. The clinical uses indicated in the table represent both on and off-label uses of beta-blockers. For example, a beta-blocker may only be approved by the FDA for treatment of hypertension; however, physicians sometimes elect to prescribe the drug for angina because of the class-action benefit that beta-blockers have for angina.
| Clinical Uses | ||||||
| Class/Drug | HTN | Angina | Arrhy | MI | CHF | |
| Non-selective β1/β2 | ||||||
| carvedilol | X | X | ||||
| MSA; additional alpha-blocking activity | ||||||
| labetalol | X | X | ||||
| ISA; MSA; additional alpha-blocking activity | ||||||
| nadolol | X | X | X | X | ||
| long acting | ||||||
| penbutolol | X | X | ||||
| ISA | ||||||
| pindolol | X | X | ||||
| ISA; MSA | ||||||
| propranolol | X | X | X | X | ||
| MSA; prototypical beta-blocker | ||||||
| sotalol | X | |||||
| several other significant mechanisms | ||||||
| timolol | X | X | X | X | ||
| primarily used for glaucoma | ||||||
| Class/Drug | HTN | Angina | Arrhy | MI | CHF | |
| β1-selective | ||||||
| acebutolol | X | X | X | |||
| ISA; MSA | ||||||
| atenolol | X | X | X | X | ||
| betaxolol | X | X | X | |||
| MSA | ||||||
| bisoprolol | X | X | X | X | ||
| esmolol | X | X | ||||
| ultra-short acting; surgical and post-surgical HTN | ||||||
| metoprolol | X | X | X | X | X | |
| nebivolol | X | |||||
| relatively selective in most patients; vasodilating (stimulates NO release) | ||||||
| Class/Drug | HTN | Angina | Arrhy | MI | CHF | |
Abbreviations: HTN, hypertension; Arrhy, arrhythmias; MI, myocardial infarction; CHF, congestive heart failure; ISA, intrinsic sympathomimetic activity; NO, nitric oxide.
Side Effects and Contraindications
Cardiovascular side effects
Many of the side effects of beta-blockers are related to their cardiac mechanisms and include bradycardia, reduced exercise capacity, heart failure, hypotension, and atrioventricular (AV) nodal conduction block. Beta-blockers are therefore contraindicated in patients with sinus bradycardia and partial AV block. The side effects listed above result from excessive blockade of normal sympathetic influences on the heart. Considerable care needs to be exercised if a beta-blocker is given with cardiac selective calcium-channel blockers (e.g., verapamil) because of their additive effects in producing electrical and mechanical depression. Although this may change with future clinical trials on safety and efficacy of beta-blockers in heart failure, at present only carvedilol, bisoprolol, and metoprolol have been approved by the FDA for this indication.
Other side effects
Bronchoconstriction can occur, especially when non-selective beta-blockers are administered to asthmatic patients. Therefore, non-selective beta-blockers are contraindicated in patients with asthma or chronic obstructive pulmonary disease. Bronchoconstriction occurs because sympathetic nerves innervating the bronchioles normally activate β2-adrenoceptors that promote bronchodilation. Beta-blockers can also mask the tachycardia that serves as a warning sign for insulin-induced hypoglycemia in diabetic patients; therefore, beta-blockers should be used cautiously in diabetics.
Revised 11/29/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)